这是由国家癌症中心主导的一项大规模人口调查研究,纳入中国五大食管癌高发区域的人口数据,包括河北磁县、河南林州、山东肥城、江苏扬中和四川盐亭。这五个区域的食管癌发病率介于35.52/10万人~81.23/10万人,而2015年中国总体食管癌发病率约为17.87/10万。
Background:
Family clustering of esophageal cancer (EC) has been found in high-risk areas of China. However, the relationships between cancer family history and esophageal cancer and precancerous lesions (ECPL) have not been comprehensively reported in recent years. This study aimed to provide evidence for identification of high-risk populations.
Methods:
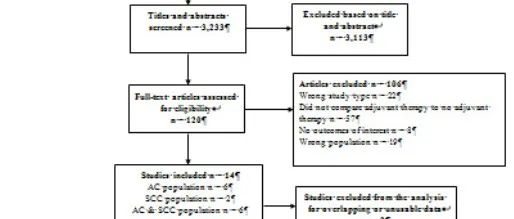
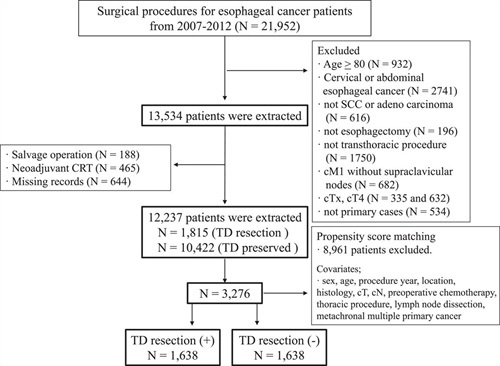
This study was conducted in five high-risk areas in China from 2017 to 2019, based on the National Cohort of Esophageal Cancer. The permanent residents aged 40 to 69 years were examined by endoscopy, and pathological examination was performed for suspicious lesions. Information on demographic characteristics, environmental factors, and cancer family history was collected. Unconditional logistic regression was applied to evaluate odds ratios between family history related factors and ECPL.
Results:
Among 33,008 participants, 6143 (18.61%) reported positive family history of EC. The proportion of positive family history varied significantly among high-risk areas. After adjusting for risk factors, participants with a family history of positive cancer, gastric and esophageal cancer or EC had 1.49-fold (95% confidence interval [CI]: 1.36–1.62), 1.52-fold (95% CI: 1.38–1.67), or 1.66-fold (95% CI: 1.50–1.84) higher risks of ECPL, respectively. Participants with single or multiple first-degree relatives (FDR) of positive EC history had 1.65-fold (95% CI: 1.47–1.84) or 1.93-fold (95% CI: 1.46–2.54) higher risks of ECPL. Participants with FDRs who developed EC before 35, 45, and 50 years of age had 4.05-fold (95% CI: 1.30–12.65), 2.11-fold (95% CI: 1.37–3.25), and 1.91-fold (95% CI: 1.44–2.54) higher risks of ECPL, respectively.
Conclusions:
Participants with positive family history of EC had significantly higher risk of ECPL. This risk increased with the number of EC positive FDRs and EC family history of early onset. Distinctive genetic risk factors of the population in high-risk areas of China require further investigation.
研究筛查了63,415名的诊疗信息,基于家族史和诊疗信息是否完善进行筛选,最终纳入研究对象33,008名。其中2,307名(6.99%)诊断为低级别上皮内瘤变/高级别上皮内瘤变/食管癌而被划分为阳性病例组;
相应的,30,701(93.01%)被诊断为正常食管/食管炎/基底细胞增生而被划分为阴性对照组。
研究以目标人群是否罹患食管癌及其癌前病变(esophageal cancer and precancerous lesions,ECPL)为目标事件。
在调整风险因素后,家族史对个人罹患ECPL的风险影响为:
恶性肿瘤家族史——1.49倍;
胃癌家族史——1.52倍;
食管癌家族史——1.66倍。
在食管癌家族史中,罹患亲属亲疏远近及个数也有影响:
单个一级亲属患食管癌,则本人患ECPL风险高1.65倍;
多个一级亲属患食管癌,则本人患ECPL风险高1.93倍。
而且,一级亲属患癌年龄越小,本人罹患ECPL风险越高。
在总体人群中,一级亲属得食管癌年龄不足35岁的,其本人罹患ECPL风险高4.05倍。
原文链接:http://www.xxwk.net/archives/1248