Purpose
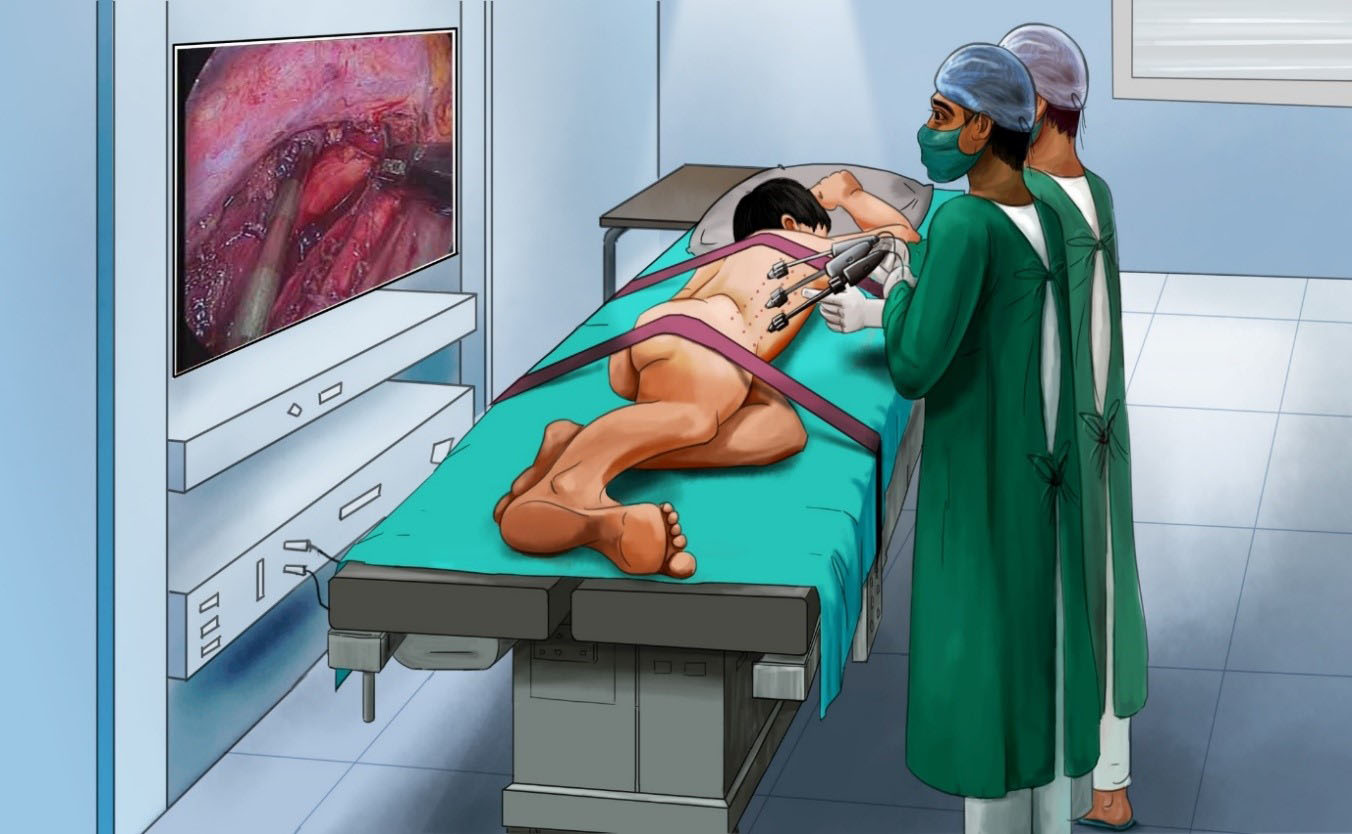
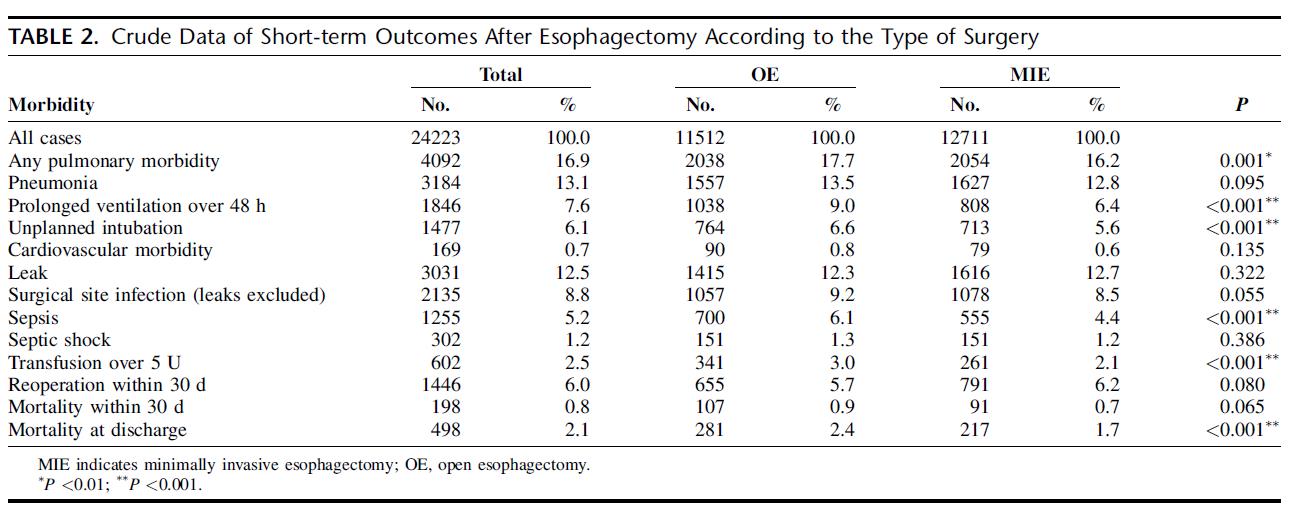
Minimally invasive esophagectomy is increasingly performed for esophageal or gastroesophageal junctional cancer, with advantages of improved perioperative outcomes in comparison with open esophagectomy. McKeown and Ivor Lewis are widely used procedures of minimally invasive esophagectomy, and there have been controversies on which one is preferred for patients with resectable esophageal or junctional cancer.
Patients and methods
This review was registered at the International Prospective Register of Systematic Reviews (number CRD42017075989). Studies in PubMed, Embase, Web of Science, the Cochrane Library, and ClinicalTrials.gov were thoroughly investigated. Eligible studies included prospective and retrospective studies evaluating short-term outcomes of minimally invasive McKeown esophagectomy (MIME) vs minimally invasive Ivor Lewis esophagectomy (MILE) in patients with resectable esophageal or junctional tumors. Main parameters included anastomotic leak and 30-day/in-hospital mortality. Overall incidence rates (ORs)/weighted mean difference (WMD) with 95% confidence intervals (CIs) were calculated by employing random-effects models.
Results
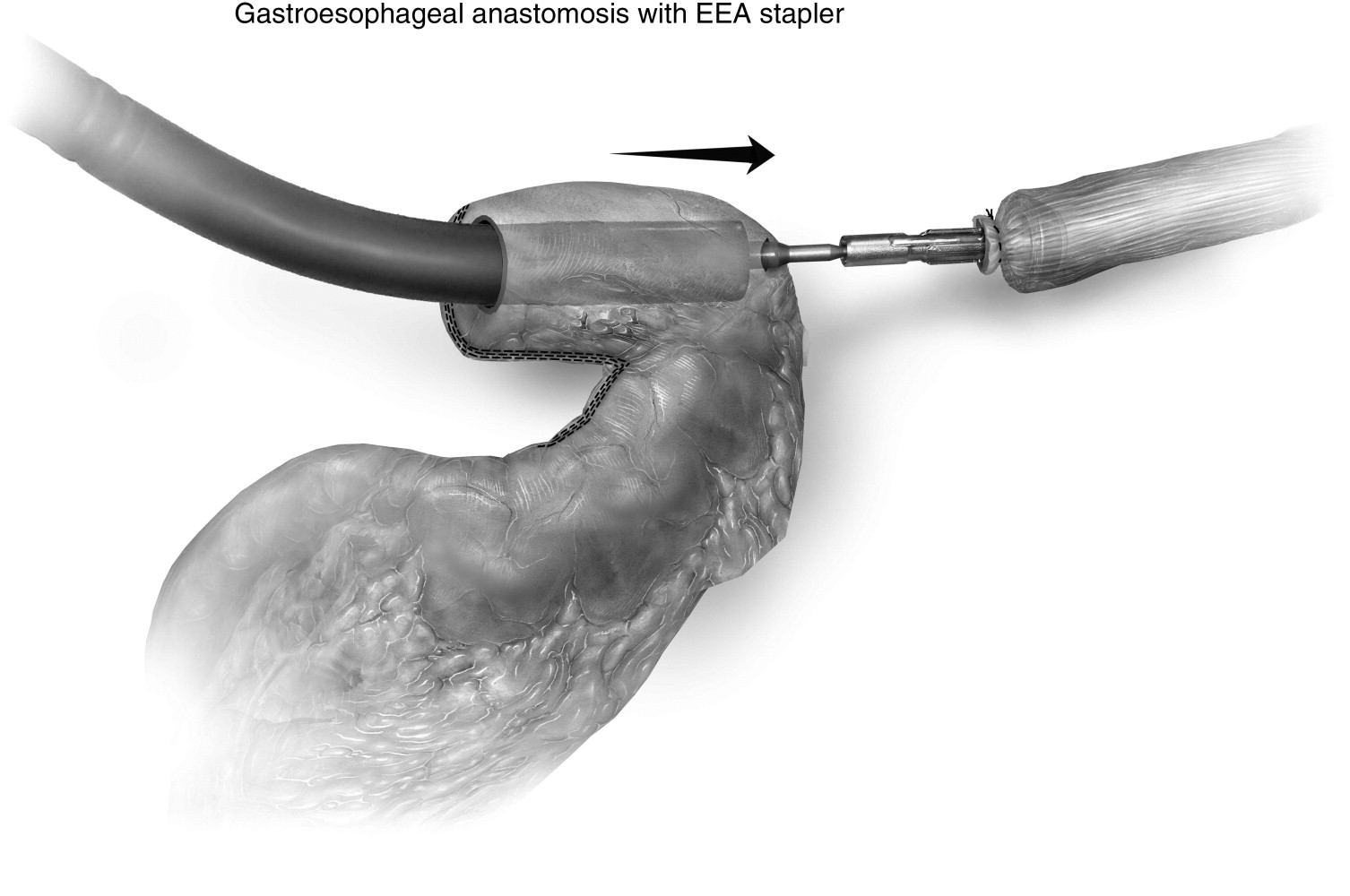
Fourteen studies containing 3,468 cases were included in this meta-analysis. Age, male sex, and American Joint Committee on Cancer (AJCC) stage between the 2 groups were not statistically different. MIME led to more blood loss, longer operating time, and longer hospital stay than MILE. MIME was associated with higher incidence of pulmonary complications (OR =1.96, 95% CI =1.28–3.00) as well as total anastomotic leak (OR =2.55, 95% CI =1.40–4.63), stricture (OR =2.07, 95% CI =1.05–4.07), and vocal cord injury/palsy (OR =5.62, 95% CI =3.46–9.14). In addition, the differences of R0 resection rate, number of lymph modes retrieved, blood transfusion rate, length of intensive care unit stay, incidence of cardiac arrhythmia, and Chyle leak between MIME and MILE were not statistically significant. Notably, incidence of severe anastomotic leak (OR =1.28, 95% CI =0.73–2.24) and 30-day/in-hospital mortality (OR =1.76, 95% CI =0.92–3.36) as well as 90-day mortality (OR =2.22, 95% CI =0.71–6.98) between the 2 procedures were also not significantly different.
Conclusion
This study suggests that MIME and MILE are comparable with respect to clinical safety. MILE may be a better option when oncologically and clinically suitable. MIME is still a safe alternative procedure when clinically indicated. However, this evidence is at risk for bias; randomized controlled trials are needed to validate or correct our results.
简介: 全微创食管切除术(TMIE)越来越多地用于治疗食管癌患者。然而,目前尚不清楚 McKeown TMIE 或 Ivor Lewis TMIE 是否应该优先用于两种手术在肿瘤学上可行的患者。
方法: 该研究于 2009 年 11 月至 2017 年 4 月期间在 4 个高容量的荷兰食管癌中心进行。前瞻性收集了来自接受 McKeown TMIE 或 Ivor Lewis TMIE 的位于食管远端或胃食管交界处的连续食管癌患者的数据。患者的倾向评分与年龄、体重指数、性别、美国麻醉医师协会分类、查尔森合并症指数、肿瘤类型、肿瘤位置、临床分期、新辅助治疗和手术医院相匹配。主要结果参数是需要再次干预或再次手术的吻合口漏。次要结果参数是手术特征、病理结果、并发症、再干预、再手术、住院时间和死亡率。
结果: 在所有纳入的 787 名患者中,匹配后仍有 420 名患者。McKeown TMIE 后需要再次介入或再次手术的吻合口漏发生率为 23.3%,而 Ivor Lewis TMIE 后为 12.4% (P = 0.003)。Ivor Lewis TMIE 与肺部并发症(46.7% 对 31.9%)、喉返神经麻痹(9.5% 对 0.5%)、再手术(18.6% 对 11.0%)、90 天死亡率(7.1% 对2.9%),重症监护病房中位住院时间较短(2 天 vs 1 天)和住院时间中位数较短(12 天 vs 11 天)(所有 P < 0.05)。各组之间的 R0 切除率相似。McKeown TMIE 后检查的淋巴结中位数为 21,Ivor Lewis TMIE 后为 25(P < 0.001)。
结论: 在两种手术在肿瘤学上可行的患者中,与 McKeown TMIE 相比,Ivor Lewis TMIE 与较低的吻合口漏发生率、90 天死亡率和其他术后发病率相关。
原文链接:http://www.xxwk.net/archives/509