Background: Although neoadjuvant therapy followed by surgery (NT) is the standard of care for esophageal cancer in Western countries, upfront surgery (US) followed by adjuvant therapy (when indicated) still is commonly used in Asia to minimize overtreatment. This study investigated the cost-effectiveness of NT versus US for patients with esophageal squamous cell carcinoma (ESCC).
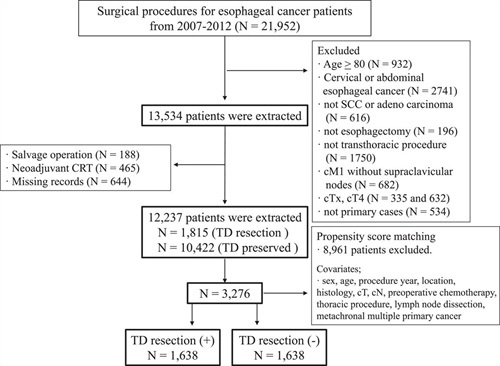
Methods: Patients with a diagnosis of ESCC between 2010 and 2015 were divided into NT or US according to the intention to treat. Two propensity score-matched groups of patients with clinical stage 2 (135 pairs) or stage 3 (194 pairs) disease were identified and compared in terms of overall survival (OS) and direct costs incurred within 3 years after diagnosis.
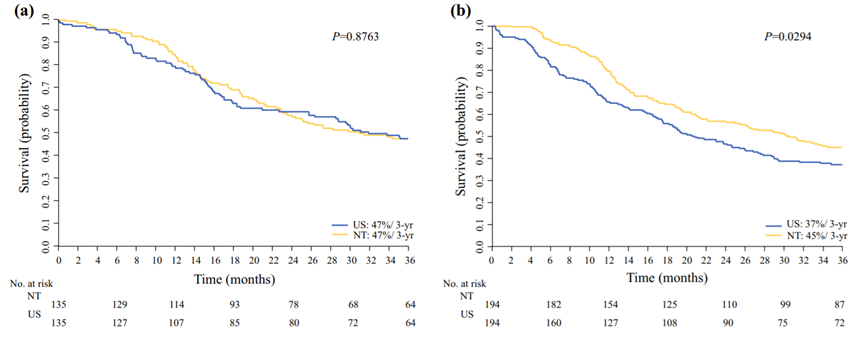
Results: The esophagectomy rates after NT were 82% for stage 2 and 88% for stage 3 disease. Compared with US, surgery after NT was associated with higher R0 resection rates, a lower number of dissected lymph nodes, and similar postoperative mortality. On an intention-to-treat analysis, stage 3 patients who received NT had a significantly better 3-year OS rate (45%) than those treated with US (37%) (p = 0.029) without significant cost increases (p = 0.89). However, NT for clinical stage 2 disease neither increased costs nor improved 3-year OS rates (47% vs 47%; p = 0.88). At a willingness-to-pay level of US$50,000 per life-year, the probability of NT being cost-effective was 92% for stage 3 versus 59% for stage 2 ESCC.
Conclusion: Because of its higher cost-effectiveness, NT is preferable to US for patients with clinical stage 3 ESCC, but US remains a viable option for stage 2 disease.
尽管在西方国家,新辅助治疗(NT)序贯手术是局部晚期食管癌的标准治疗,但在亚洲国家,为了减少过度治疗,手术联合必要的辅助治疗(US)仍被广泛应用,尤其是对于临床分期较早的患者。为了探索临床2~3期食管鳞癌(ESCC)患者NT与US两种治疗模式的成本-效益,中国台湾长庚大学长庚纪念医院胸外科的学者开展了此项真实世界研究,近日在线发表于《外科肿瘤学年鉴》(Annals of Surgical Oncology)。
研究者表示,这应是目前首个提供NT对比US成本-效益真实世界证据的研究。结果显示,对于临床3期ESCC患者,NT模式较US模式的成本-效益更优,而对于2期患者,US模式仍为可选方案。
研究将中国台湾癌症登记数据库中2010-2015年间治疗的ESCC确诊病例,根据治疗方式分为NT组和US组。经倾向评分匹配,临床2期和临床3期队列分别配成135对和194对。
临床2期和3期队列中,NT后食管切除率分别为82%和88%;与US组相比,NT组具有更高的R0切除率、更少的淋巴结清扫数目和相似的术后死亡率,两个分期队列中均是如此。
在意向性治疗(ITT)分析中,3期患者NT组的3年OS率显著优于US组(45% vs. 37%,P=0.029),且未显著增加治疗花费(P=0.89)。然而,在2期患者中,NT组较US组虽未增加治疗花费,但也未显著改善3年OS率(47% vs. 47%,P=0.88)。见图3。在每生命年50000美元的治疗支出水平上,对于3期和2期ESCC患者,NT成本-效益有利的概率分别为92%和59%。
相较于NT模式,US模式的一项潜在优势为,术后能够获得准确的病理学数据,从而为辅助治疗决策提供更可靠的依据。这能够使过度治疗风险最小化,避免因临床过度分期所致的不必要的治疗支出。但同时,如果临床分期低于实际,US模式也可能导致无益的手术切除。此外,部分患者可能因术后耐受性差不能及时接受辅助治疗,进而影响生存结局。因此,理想的方案是,在治疗花费最小或在可接受范围内的情况下,能够带来更多的疗效获益。
从本研究结果可以看到,相较于US模式,NT模式在临床3期ESCC患者中的成本-效益优势显著,但在2期患者中则不然。令人意外的是,无论何种分期,US模式都未显示出可观的成本节省,值得关注与探讨,尤其是本研究源于真实世界临床数据,理论上较随机对照试验更加符合实践中患者的治疗情况,比如本研究包含了辅助治疗的费用,也纳入了疾病进展后的治疗支出。
作者在讨论中也分析了本研究存在的局限性,包括回顾性研究固有的选择偏倚、缺乏是否进行辅助治疗的亚组分析,以及由于数据库数据的限制只能采用生命年而非质量调整寿命年(QALYs)等。
文章来源于嘉议肿瘤
原文链接:http://www.xxwk.net/archives/354