Background: After neoadjuvant chemoradiotherapy for oesophageal cancer, roughly half of the patients with squamous cell carcinoma and a quarter of those with adenocarcinoma have a pathological complete response of the primary tumour before surgery. Thus, the necessity of standard oesophagectomy after neoadjuvant chemoradiotherapy should be reconsidered for patients who respond sufficiently to neoadjuvant treatment. In this study, we aimed to establish the accuracy of detection of residual disease after neoadjuvant chemoradiotherapy with different diagnostic approaches, and the optimal combination of diagnostic techniques for clinical response evaluations.
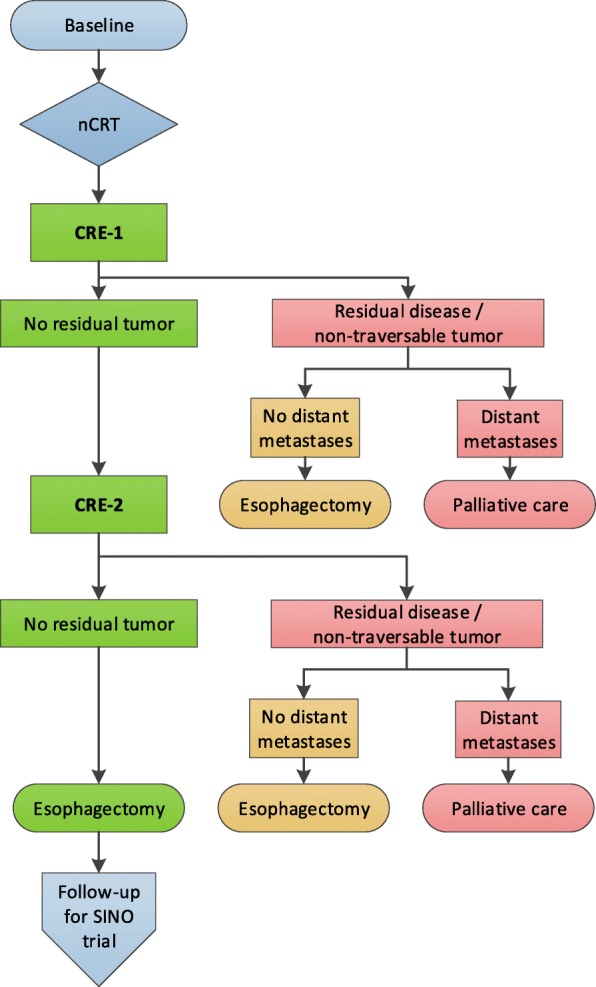
Methods: The preSANO trial was a prospective, multicentre, diagnostic cohort study at six centres in the Netherlands. Eligible patients were aged 18 years or older, had histologically proven, resectable, squamous cell carcinoma or adenocarcinoma of the oesophagus or oesophagogastric junction, and were eligible for potential curative therapy with neoadjuvant chemoradiotherapy (five weekly cycles of carboplatin [area under the curve 2 mg/mL per min] plus paclitaxel [50 mg/m2 of body-surface area] combined with 41·4 Gy radiotherapy in 23 fractions) followed by oesophagectomy. 4-6 weeks after completion of neoadjuvant chemoradiotherapy, patients had oesophagogastroduodenoscopy with biopsies and endoscopic ultrasonography with measurement of maximum tumour thickness. Patients with histologically proven locoregional residual disease or no-pass during endoscopy and without distant metastases underwent immediate surgical resection. In the remaining patients a second clinical response evaluation was done (PET-CT, oesophagogastroduodenoscopy with biopsies, endoscopic ultrasonography with measurement of maximum tumour thickness, and fine-needle aspiration of suspicious lymph nodes), followed by surgery 12-14 weeks after completion of neoadjuvant chemoradiotherapy. The primary endpoint was the correlation between clinical response during clinical response evaluations and the final pathological response in resection specimens, as shown by the proportion of tumour regression grade (TRG) 3 or 4 (>10% residual carcinoma in the resection specimen) residual tumours that was missed during clinical response evaluations. This study was registered with the Netherlands Trial Register (NTR4834), and has been completed.
Findings: Between July 22, 2013, and Dec 28, 2016, 219 patients were included, 207 of whom were included in the analyses. Eight of 26 TRG3 or TRG4 tumours (31% [95% CI 17-50]) were missed by endoscopy with regular biopsies and fine-needle aspiration. Four of 41 TRG3 or TRG4 tumours (10% [95% CI 4-23]) were missed with bite-on-bite biopsies and fine-needle aspiration. Endoscopic ultrasonography with maximum tumour thickness measurement missed TRG3 or TRG4 residual tumours in 11 of 39 patients (28% [95% CI 17-44]). PET-CT missed six of 41 TRG3 or TRG4 tumours (15% [95% CI 7-28]). PET-CT detected interval distant histologically proven metastases in 18 (9%) of 190 patients (one squamous cell carcinoma, 17 adenocarcinomas).
Interpretation: After neoadjuvant chemoradiotherapy for oesophageal cancer, clinical response evaluation with endoscopic ultrasonography, bite-on-bite biopsies, and fine-needle aspiration of suspicious lymph nodes was adequate for detection of locoregional residual disease, with PET-CT for detection of interval metastases. Active surveillance with this combination of diagnostic modalities is now being assessed in a phase 3 randomised controlled trial (SANO trial; Netherlands Trial Register NTR6803).
原文链接:http://www.xxwk.net/archives/496